This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
Date of admission: 21/06/22
CHIEF COMPLAINT:
A male patient aged 36 years came to the opd with chief complaints of
- Fever since 15 days
- Weakness of b/l upper and lower limbs since 3 days
HISTORY OF PRESENT ILLNESS:
Patient came to the casuality with altered sensorium and quadriparesis.
Patient was apparently asymptomatic 15 days back, then he presented with fever which was intermittent and relieved on medication.
Patient had complaints of weakness of b/l upper limb and lower limb with decrease in tone and power since 3 days.
Patient also had developmental delay of milestones in his childhood ( he walked at 6 years)
Patient also had slurring of speech since 6 years of age
Patient attained fine motor skills at the age 2 years, hearing and vision are normal since birth.
HISTORY OF PAST ILLNESS:
K/c/o Epilepsy ( since 6 months of age)
Not a k/c/o HTN, DM , TB , CAD , asthma
TREATMENT HISTORY:
No relevant treatment history
PERSONAL HISTORY:
- Appetite is normal
- Having mixed diet
- Bowels regular
- Micturition normal
- Alcohol - teetotaler
- No habit of smoking
- No other habits/ addictions
GENERAL EXMINATION:
Patient is conscious, coherent
Presence of pedal edema( non pitting edema)
Absence of pallor, icterus, clubbing, cyanosis, lymphadenopathy.
VITALS:
1.Temperature: 101 F
2.Pulse rate: 100 beats per min
3.Respiratory rate: 20 cycles per min
4.BP: 150/80mm Hg
5.SpO2: 98% @Room air
6.GRBS: 156mg %
SYSTEMIC EXAMINATION:
CARDIOVASCULAR SYSTEM:
- S1, S2 heard
- No thrills, No murmurs
RESPIRATORY SYSTEM:
- Normal vesicular breath sounds
- Position of trachea is central
- Dyspnea is absent
- No wheeze
EXAMINATION OF ABDOMEN:
- Shape of abdomen - scaphoid
- No tenderness
- No palpable mass
- Normal hernial orifices
- No free fluid
- No Bruits
- Liver is not palpable
- spleen is not palpable
- Bowel sounds heard
CENTRAL NERVOUS SYSTEM:
- Patient is conscious
- Altered sensorium
- Quadriparesis
RT LT
TONE: UL hypotonia hypotonia LL hypotonia. hypotonia
POWER: UL 2/5 2/5
LL 0/5 0/5
REFLXES: B ++ ++
T ++ ++
S ++ ++
K ++ ++
A ++ ++
P Flexion Flexion
PROVISIONAL DIAGNOSIS:
Fever with altered sensorium
Sepsis
Leptospirosis+
Quadriparesis secondary to AMSAN
Myositis
AKI ( ? pre renal)
Intellectual disability
? Viral encephalitis
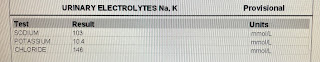
INVESTIGATIONS:
ECG
MRI report
CHEST X-RAY
TREATMENT:
On 21/06/22:
1. INJ. MONOCEF 2gm/IV/BD
2. INJ. DEXA 8mg/IV/TID
3. INJ. DOXY 100mg/IV/BD
4. IVF ONS @ 50ml/hr
ORL
5. INJ. PAN 40mg/IV/OD
6. TAB DOLO 650mg/RT/TID
7. INJ. NEOMOL 1gm/IV/SOS
8. Tepid sponging
9. GRBS charting 6th hrly
10. Monitor vitals 1hrly
11. Temp charting 1 hrly
On 22/06/22:
1. INJ. Falcigo 120mg/IV/stat
2. INJ. Acyclovir 500mg/IV/TID
3. INJ. MONOCEF 2gm/IV/BD
4. INJ. DEXA 8mg/IV/TID
5. INJ. DOXY 100mg/IV/BD
6. IVF ONS @ 50ml/hr
RL
7. INJ. PAN 40mg/IV/OD
8. TAB DOLO 650mg/RT/TID
9. INJ. NEOMOL 1gm/IV/SOS
10. Tepid sponging
11. GRBS charting 6th hrly
12. Monitor vitals 1hrly
13. Temp charting 1 hrly






























Comments
Post a Comment