GENERAL MEDICINE E-LOG
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
CHIEF COMPLAINT:
A 24 year old female came to the opd with chief complaints of
- Fever
- Vomitings and
- Bloating since 3 days
Patient was apparently asymptomatic 3 days back, then she developed fever associated with chills and rigor( subsided on taking medication). Fever was present throughout the day which was of Intermittent type with no diurnal variation.
She had complaints of bloating followed by vomitings ( 3 episodes in a day) which had food particles as content.
No bleeding manifestation
No c/o burning micturition
No c/o cough, cold, headache, pedal edema
Patient was taken to the near by RMP doctor was told her platelet count was low and was referred to our hospital.
HISTORY OF PAST ILLNESS:
Not a k/c/o DM, Hypertension, Asthma, TB, epilepsy.
No similar complaints in the past.
TREATMENT HISTORY:
NO relevant treatment history
PERSONAL HISTORY:
- Married for 3 years
- Appetite is normal and improved
- Having mixed diet( Non vegetarian)
- Bowels- Regular
- Micturition- Normal
- No other habits/addictions
Pallor is present.
Absence of Icterus, Clubbing, Cyanosis, Pedal edema, Lymphadenopathy.
VITALS:
1.Temperature: 98.6 F
2.Pulse rate: 84 beats per min
3.Respiratory rate: 18 cycles per min
4.BP: 100/80 mm Hg
5.SpO2: 99% @ Room air
6.GRBS: 106mg%
SYSTEMIC EXAMINATION:
CARDIOVASCULAR SYSTEM:
- S1, S2 heard
- No thrills, No murmurs
- Normal vesicular breath sounds
- Position of trachea is central
- Dyspnoea is absent
- No wheeze
- Shape- scaphoid
- Tenderness is present in right hypochondriac region
- No palpable pass
- Normal hernial orifices
- No free fluid
- No Bruits
- Liver is not palpable
- spleen is not palpable
- Bowel sounds heard
- Patient is conscious
- Speech is normal
- No focal neurological defect
VIRAL PYREXIA WITH THROMBOCYTOPENIA
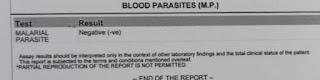
INVESTIGATIONS:
Investigations on 13/08/21:
chest X-Ray
ECG







Comments
Post a Comment