A 31yr old male with Alcoholic Liver Disease
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E-LOG was done under the guidance of Dr. Madhumitha
CHIEF COMPLAINT:
A 31 year old male came to the opd with chief complaints of
- Abdominal pain and distension since 7 days
- Pedal edema extending upto knees since 7 days
- Fever since 4 days
HISTORY OF PRESENT ILLNESS:
Patient was apparently asymptomatic 1 year back then he had pain in abdomen which is of diffuse type(Not associated with vomiting).
He stopped drinking due to the pain and got treated from local RMP for the pain.
After the pain has subsided, ,he started to drink again. He had multiple attacks of pain in the abdomen during the past 1 year.
Two months back he had c/o yellowish discoloration of eyes, pain in the abdomen and b/l pedal edema for which he got treated at NIMS, his symptoms subsided within 2 days.
Then he was tested positive for COVID-19 by RTPCR test, for which he referred to Gandhi hospital and took medication for 10 days and went back home. By that time yellowish discoloration of eyes was still present.
One week back he had non-vegetarian food(mutton) for his dinner, and then developed pain in the abdomen, for which he got treated in the local hospital.
There was insidious onset of Abdominal distension, pedal edema extending upto knees and Fever(Intermitent, low grade, relieved with medication) since 4 days.
HISTORY OF PAST ILLNESS:
Not k/c/o DM, hypertension, asthma, epilepsy, Heart disease or tuberculosis.
He has a treatment history which has been taken for RTA which occurred twice once in 2007 and 2014, where he got treated for head injury in both the cases in 2 different hospitals.
No treatment history for DM, hypertension, asthma, epilepsy, Heart disease or tuberculosis.
PERSONAL HISTORY:
He has been consuming alcohol 180ml/day and smoking 1 pack of cigarette/day since past 10 years.
He had an abstinence from alcohol since 2 months.
GENERAL EXAMINATION:
Patient is conscious.
Icterus is present.
B/L Pedal edema is present.
Absence of pallor, cyanosis, clubbing, lymphadenopathy.
VITALS:
1.Temperature:- 98.4 F
2.Pulse rate: 84 beats per min
3.Respiratory rate: 24 cycles per min
4.BP: 80/60 mm Hg
5.SpO2: 98% @ Room air
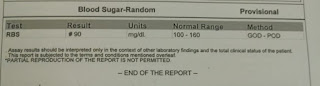
6.GRBS: 126mg%
SYSTEMIC EXAMINATION:
CVS:
- S1,S2 heard, no murmurs.
- Normal vesicular breath sounds.
- Abdomen is distended
- No tenderness
- No focal neurological defect.
Course in the hospital:
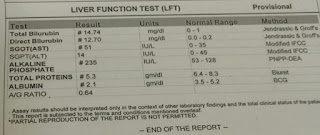
This is a case of 31 year old male with Chronic Liver Disease with Grade 1 varices with Acute Kidney Injury. Patient was admitted on 14/07/2021. Diagnostic ascitic tap of 1 litre was done and the ascitic fluid was sent for investigation which showed high SAAG and low protein. UGIE showed Grade 1 varices with low grade portal HTN and mild PHG. Patient was treated with Inj. Vit k 10mg, Tab Udiliv 300mg, Tab Rifaximine 550mg, Syp. Hepamerz 10ml, Syp Lactulose, Tab Lasix 20mg, Tab Aldactone 25mg everyday and was advised discharge on 19/7/21.
Advice at Discharge:
1. Tab. Udiliv 300mg PO/BD
2. Tab. Lasix 20mg PO/BD
3. Tab Aldactone 25mg PO/BD
4. Syp Hepamerz 10ml TID
5. Syp Lactulose 15ml
]\













Comments
Post a Comment